from the Richmond Fed
— this post authored by Jessie Romero
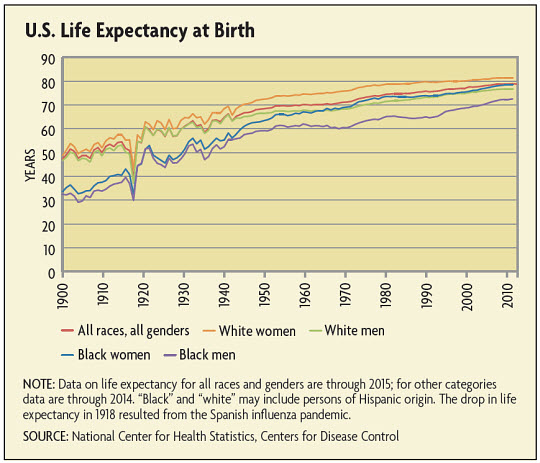
At the turn of the 20th century, most babies born in America could expect to die before age 50 – if they survived past their first birthday, which roughly one in 10 babies did not. But over the past century, improvements in sanitation, nutrition, and medical care – especially the development of vaccines and antibiotics – have driven a dramatic increase in life expectancy. Babies born today can expect to live until they are nearly 80, and adults who reach old age are increasingly likely to survive additional years.

But between 2014 and 2015, life expectancy for the U.S. population as a whole declined for the first time in more than two decades; some research suggests the decline has been more pronounced, and perhaps has been a longer-term trend, for whites (that is, non-Hispanic whites). In addition, while it has long been the case that the wealthier and more educated have had longer life expectancies and lower mortality rates than those with less money and education, the gap appears to have grown in recent decades.
The magnitude of changes in life expectancy and “mortality inequality” is the subject of considerable debate, as are the causes. But to the extent life expectancies have stagnated or declined, “I do think we should be concerned,” says economist Janet Currie of Princeton University. “It suggests that things are going wrong for certain people.”
Recent Trends in Life Expectancy
Between 1900 and 2014, life expectancy at birth in the United States increased nearly 70 percent, from 47.3 years to 78.9 years. (See chart below.) But in 2015, life expectancy declined to 78.8 years – only a slight drop, but the first since 1993, when death rates spiked due to the AIDS pandemic and a particularly lethal flu season. The decline was reported in a December 2016 report by the Centers for Disease Control (CDC).
Life expectancy at birth tends to understate the number of years an individual is actually likely to live. The measure denotes the average age infants born in a given year can expect to reach, assuming the mortality trends prevailing at the time of their birth prevail for their entire lives. But life expectancy generally increases as people reach older ages. That’s in part because, historically, mortality trends have improved over time, and in part because life expectancy at a given age is conditional on having reached that age. For example, a white baby girl born in 1949 had, at that time, a life of expectancy of about 72 years. But by the time that baby was 65, in 2014, she could expect to live about 20 more years, to age 85.
The 2015 decline in life expectancy was driven by increases in mortality rates of white men and women of 1 percent and 1.6 percent, respectively, and an increase of 0.9 percent for black men (that is, non-Hispanic black men). This decline follows a drop in life expectancy for whites from 78.9 years in 2013 to 78.8 years in 2014, the most recent year for which the CDC has published life tables by race and ethnicity. The 2014 decrease was driven by a decline among white women from 82.2 years to 81.1 years. (Life expectancy was unchanged for white men at 76.5 years.)
Are More White People Dying?
While it’s possible the recent decline for the population as a whole is just a statistical blip, there is some evidence that changes in mortality for whites in particular might be more persistent.
In a recent article, Anne Case and Angus Deaton of Princeton University analyzed mortality rates for U.S. adults. They found that between 1978 and 1998, the mortality rate for non-Hispanic whites aged 45-54 declined about 2 percent per year on average. But between 1999 and 2013, the mortality rate for this group increased about half a percent per year even as mortality rates for other racial and ethnic groups continued to decline. According to their calculations, had the mortality rate for whites in this age group remained at its 1998 level, nearly 100,000 fewer people would have died; had the rate continued its previous rate of decline, nearly 500,000 fewer lives would have been lost.
Case and Deaton noted that the increase in white mortality they observed was concentrated in individuals with less education. Similarly, in a 2012 article in the journal Health Affairs, a team of researchers found large and unprecedented declines in life expectancy for non-Hispanic whites who had not graduated from high school. Between 1990 and 2008, life expectancy at birth for white women without a high school degree fell by more than five years; for men, the drop was more than three years. Life expectancy for blacks and Hispanics with less than a high school diploma continued to increase during this period.
But it’s possible that the magnitude of this decline for white high school dropouts was simply the result of changes in the composition of the group of people who have not graduated from high school. Educational attainment for the population as a whole increased significantly over the course of the 20th century. As a result, cohorts of people who have not completed high school have become smaller – and perhaps more disadvantaged – over time.
“Not finishing high school when this is the norm means that those in this group likely had some underlying background or characteristics working against them, such as a high level of disadvantage growing up, early life poor health, or a lack of aptitude for school,” explains Jennifer Dowd of King’s College London and the City University of New York School of Public Health. “It could be the case that they have become more disadvantaged, or it could be that they are as disadvantaged as always, but now they’re not being averaged into the group with better outcomes.” Either way, Dowd says, comparing groups of people who have not completed high school decades apart is akin to “making an apples to oranges comparison over time, but calling both fruits apples.”
One way to address the problem is to measure relative rather than absolute educational attainment, as John Bound and Arline Geronimus of the University of Michigan, Javier Rodriguez of Mathematica Policy Research, and Timothy Waidmann of the Urban Institute did in a 2015 article. They found that life expectancy for white women in the bottom quartile of the distribution fell 1.2 years between 1990 and 2010, and white men in this quartile experienced a slight increase. (Black and Hispanic life expectancy might be less affected by compositional changes because a larger proportion of blacks and Hispanics do not complete high school, although completion rates for these groups have increased.)
Compositional changes might also have played a role in Case and Deaton’s findings. Over the period they studied, the baby boom generation began moving into the 45-54 age group, and the average age of the group increased from 49.3 years to 49.7 years. While this is a relatively small increase, mortality rates increase substantially with age, which could bias a comparison of age-group mortality over time. Andrew Gelman of Columbia University calculated age-adjusted mortality rates for non-Hispanic whites in this age group and found an increase between 1999 and 2005 and a flattening between 2005 and 2013 – a less dramatic reversal than found by Case and Deaton, albeit still a notable break from the previous trend and from the mortality patterns experienced by other groups. Gelman also found differences by gender: Mortality for non-Hispanic white men increased until 2005, and then began to decline again. But the mortality rate for non-Hispanic white women increased steadily over the period studied.
In a 2016 article in the Journal of Economic Perspectives, Currie and Hannes Schwandt of the University of Zurich compared life expectancies and mortality rates by race, gender, and socioeconomic status as measured by county poverty rates. They also found a divergence in mortality patterns for white women. Between 1990 and 2010, mortality rates for all white women aged 20-49 were essentially unchanged, and even increased slightly for women in the poorest counties, compared with continued declines in mortality for other groups. But, Currie notes, it’s not all bad news. “Changes to life expectancy for middle-aged white women have been very small and from a low base. At the same time, the gains in life expectancy for young African-American men have been huge over the past 20 years and dwarf those changes.”
Long Live the Rich and Well Educated
Although the mortality rate for non-Hispanic black men ticked up in 2015, in general blacks have experienced large gains in life expectancy, leading to a considerable narrowing of the racial gap. In 1900, white life expectancy was 14 years longer than black life expectancy; by 1970, the gap was seven years, and in 2014, it had fallen to three years. Hispanics tend to have longer life expectancy than both whites and blacks, despite the fact that they tend to be of lower socioeconomic status. (See sidebar below.)
A large body of research, dating back to the seminal 1973 book Differential Mortality in the United States by Evelyn Kitagawa and Philip Hauser, has documented lower mortality rates and longer life expectancy for people with more income and more education. While estimates vary, studies suggest that a 25-year-old man with a high school diploma can expect to live between two and seven years longer than a man without a high school diploma; the gap for women is between two and six years.
While gender and racial gaps in life expectancy have narrowed, socioeconomic ones have increased. Between the 1980s and 2000, the gap in life expectancy between those with at least some college and those with a high school diploma or less increased by about 30 percent, according to research by Ellen Meara of Dartmouth College, Seth Richards-Shubik of Lehigh University, and David Cutler of Harvard University. (The authors controlled for negative selection by equalizing the share of individuals in the high- and low-education groups.)
Bound, Geronimus, Rodriguez, and Waidmann also found an increase in the education gap when measuring by relative educational attainment: Between 1990 and 2010, whites in the top three quartiles of the education distribution had much larger gains in life expectancy than those in the bottom quartile.
Similar trends are apparent when comparing life expectancy by income level. In a 2007 article, Hilary Waldron, an economist at the Social Security Administration, found that among men born in 1912 who survived to age 60, those in the top half of the income distribution could expect to live 1.2 years longer than those in the bottom half. For men born in 1941, the gap had increased to 5.8 years. (Waldron’s data were for male Social Security-covered workers.) More recently, Raj Chetty of Stanford University and several co-authors studied life expectancy trends between 2001 and 2014. They found that life expectancy at age 40 increased 2.3 years during that period for men in the top 5 percent of the income distribution but only 0.3 years for men in the bottom 5 percent. High-income women gained 2.9 years in life expectancy, while gains for low-income women were negligible.
Waldron’s and Chetty’s studies focused on life expectancy at older ages. But Currie and Schwandt also studied changes in mortality inequality for children. Consistent with other research, they found that between 1990 and 2010, mortality rates for older adults decreased more in low-poverty counties than in high-poverty counties, leading to greater mortality inequality. But for children, mortality rates declined much more in poor counties than in rich ones, resulting in less inequality. Given the large body of research demonstrating that childhood health is a strong predictor of adult health, this suggests that today’s children could experience less inequality in mortality and life expectancy as adults.
A Perfect Storm
Why are today’s adults experiencing more inequality in life expectancy? Researchers have studied multiple explanations, but establishing a causal relationship between financial resources or education and mortality risk is a challenging task. In part, that’s because the relationship runs in both directions; healthier people are in a better position to work and earn higher incomes in the first place, and those in poor health might have to stop working. In addition, a link between wealth and mortality might exist if poor health reduces a person’s assets through high medical expenditures. In the other direction, those with more income and wealth are able to purchase better health care and to purchase it earlier.
With respect to education, many studies have tried to disentangle whether increasing educational disparities are the result of composition or causation. The answer, says Jennifer Karas Montez of Syracuse University, is probably a little of both. “People not graduating from high school today certainly have more disadvantaged backgrounds than people who didn’t graduate a hundred years ago,” she says. “At the same time, what it means to go out into the world today without a high school credential is much more problematic than it was a hundred years ago. So you have a perfect storm: a more disadvantaged group going out and achieving a level of education that itself confers disadvantage.”
Karas Montez adds, “There’s really nothing inherently causal about the relationship between education and mortality. The context we’re living in shapes that relationship. Do you live in an environment where education opens the door to getting a good job, to having health care, to living in a safe neighborhood? Or do you have some other initial advantages or safety net that make your own human capital less important?”
One factor in rising mortality, particularly for whites, could be the opioid crisis. Since 1999, overdose deaths from opioids, including both prescription drugs and heroin, have quadrupled, according to the CDC. The increase in opioid abuse and related deaths has been concentrated among whites, although blacks and Hispanics also have been affected. In addition, while the suicide rate has increased for the population as a whole since 2000, the increase has been much larger for whites than for blacks and Hispanics. Case and Deaton also found that death rates from suicide and alcohol-related liver disease increased for less-educated whites between 1999 and 2013 but fell or remained flat for blacks and Hispanics. Some researchers have dubbed these “deaths of despair” and suggested that increasing economic insecurity could be to blame. Still, says Currie, “African-Americans have always had higher unemployment than whites. So to see life expectancy continuing to improve for African-Americans over time casts doubt on any simple story about the health effects of economic disadvantage.”
In addition, present-day mortality patterns might reflect decisions that were actually made decades ago, such as the decision to start or quit smoking. After the surgeon general released a report on the hazards of smoking in 1964, people with more education were much more likely to quit smoking. In addition, men quit smoking more quickly than women. Less-educated white women in particular continued to start smoking even as other groups were quitting and were slower to quit themselves. And because the negative effects of smoking can manifest themselves long after a person has stopped smoking, current mortality rates could be affected.
“If you see differences in death rates between groups now, you shouldn’t necessarily jump to the conclusion that it reflects what’s happening to them right now,” says Currie. “Some of what you’re seeing are the lagged effects of things that happened a long time ago.”
On an individual level, public health initiatives targeting smoking, child health, and opioid abuse could lower mortality risk and increase life expectancy for certain groups. But at the societal level, the complicated interplay between income, education, and health makes it difficult to ascertain how or if a given social policy will affect mortality risk. Still, says Dowd, “There is clearly huge scope for understanding how the malleable parts of the human social condition can affect health. Scholars have to keep testing the health impacts of more specific education and other social policy changes to understand what works best to give all social classes the best opportunities for good health.”
Policymakers could have good reason to try to reduce mortality rates and mortality inequality. Beyond basic questions of equity and fairness, there may be implications for economic growth. Research suggests that when people expect to live longer, they invest more in their own human capital, making themselves more productive. And at the most basic level, economic growth depends on how many people are working and how productive they are: A healthier society is likely to be a wealthier society.
Readings
Bound, John, Arline T. Geronimus, Javier M. Rodriguez, and Timothy A. Waidmann. “Measuring Recent Apparent Declines in Longevity: The Role of Increasing Educational Attainment.” Health Affairs, December 2015, vol. 34, no. 12, pp. 2167-2173.
Case, Anne, and Angus Deaton. “Rising Morbidity and Mortality in Midlife among White Non-Hispanic Americans in the 21st Century.” Proceedings of the National Academy of Sciences, Dec. 8, 2015, vol. 112, no. 49, pp. 15078-15083.
Currie, Janet, and Hannes Schwandt. “Mortality Inequality: The Good News from a County-Level Approach.” Journal of Economic Perspectives, Spring 2016, vol. 30, no. 2, pp. 29-52.
Cutler, David M., Ellen R. Meara, and Seth Richards-Shubik. “The Gap Gets Bigger: Changes in Mortality and Life Expectancy, by Education, 1981-2000.” Health Affairs, March 2008, vol. 27, no. 2, pp. 350-360.
Dowd, Jennifer B., and Amar Hamoudi. “Is Life Expectancy Really Falling for Groups of Low Socio-economic Status? Lagged Selection Bias and Artefactual Trends in Mortality.” International Journal of Epidemiology, August 2014, vol. 43, no. 4, pp. 983-988. (Article available online with subscription.)
Karas Montez, Jennifer, and Anna Zajacova. “Explaining the Widening Education Gap in Mortality among U.S. White Women.” Journal of Health and Social Behavior, June 2013, vol. 54, no. 2, pp. 165-181.
Karas Montez, Jennifer, and Kaitlyn Barnes. “The Benefits of Educational Attainment for U.S. Adult Mortality: Are They Contingent on the Broader Environment?” Population Research and Policy Review, February 2016, vol. 35, no. 1, pp. 73-100. (Article available online with subscription.)
Source
https://www.richmondfed.org/publications/research/econ_focus/2016/q3-4/feature3







